Lemierre's syndrome (or suppurative thrombophlebitis of the internal jugular vein) was originally described as a complication of postanginal sepsis.1-5 Lemierre, in 1936, wrote a comprehensive article on the subject and called this syndrome “postanginal septicemia. 4
This syndrome is a rare but severe life-threatening complication of oral infections, particularly those resulting in lateral pharyngeal space infection. It is characterized as thrombosis and suppurative thrombophlebitis of the internal jugular vein that is associated with spread of septic emboli to the lungs and other sites. Before the availability of antimicrobial agents, death was the common result, unless patients were treated with surgical ligation of the vein.2,3
Microbiology
Fusobacterium is the predominate genus and Fusobacterium necrophorum is the most prevalent species. Other Fusobacteria include Fusobacterium nucleatum, Fusobacterium gonidiaforum and Fusobacterium varium. Other isolates recovered alone or in combination include pigmented Prevotella, Bacteroides spp. and Peptostreptococcus spp.6-8
Pathophysiology
The source of the infection is pharyngitis, exudative tonsillitis, peritonsillar abscess or oral procedure (i.e., tonsillectomy), which precedes the onset of septicemia. The initiating event is generally a localized infection in an area drained by the large cervical veins. Thereafter, the infection quickly progresses to cause a pathognomic triad of findings: (1) local symptoms of neck pain, torticollis, trismus, dysphagia or dysarthria ascribable to involvement of the hypoglossal, glossopharyngeal, vagus or accessory nerves; (2) development of thrombophlebitis; (3) embolic infection of the lungs, viscera, joints or brain or direct extension of the infection to the internal ear, middle ear or mastoid. Death can occur as a result of the erosion of a blood vessel wall with rupture into the mediastinum, ear or crania vault.5
Most patients with Lemierre’s syndrome are older than 10 years.7 The patients look toxic and manifest fever, sore throat, cough neck, pain, dyspnea, and arthralgia. Palpable jugular arch can be detected in about 20% of patients. Swelling and tenderness at the angle of the jaw and along the sternocleidomastoid muscle with signs of severe sepsis along with evidence of pleuropulmonary emboli, is very suggestive of thrombophlebitis of the internal jugular vein.6
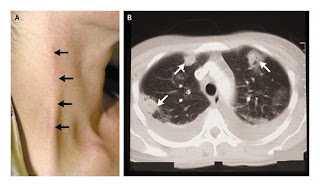
A patient with Lemierre's syndrome: A. Thropbophlebitis of external jugular vein. Bilateral pleural effusion and multiple areas of consolidation with cavitation
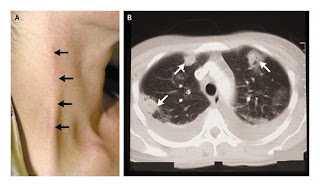 CT of a clotted jugular vein indicating Lemierre's syndrome (red arrow). A normal appearing jugular vein is indicated by the blue arrow.
CT of a clotted jugular vein indicating Lemierre's syndrome (red arrow). A normal appearing jugular vein is indicated by the blue arrow.
Pulmonary emboli are found in most untreated patients, as most present with pleuritic pain. Empyema is however rare. Seeding of other body sites occurs, mostly to the joints. Other potential sites that are involved are the liver causing “bacteremic jaundice.”8 Chest x-ray is indicated.
High resolution ultrasonography can confirm the diagnosis of suppurative thrombophlebitis.9 CT can also demonstrate intravascular thrombus; however, it is more expensive, produces higher morbidity because of intravascular contrast agents and is probably less sensitive than high resolution ultrasonography for identifying small mural thrombi.9-12 Radionuclide gallium scans can localize the source of the original infection in the internal jugular vein.13 However, inability to document a thrombus should not delay initiation of appropriate antibiotic therapy for anaerobic sepsis.
Treatment
Prolonged high dose antimicrobial therapy is important in insuring cure and preventing local and systemic extension of these infections. These agents should be directed at the eradication of the predominant organisms causing these infections. To assure that therapy is individualized, appropriate specimens should be collected from the infected site and processed for aerobic and anaerobic bacteria. The choice of the proper antibiotics depends on the antimicrobial susceptibility of the etiologic agent. Most patients respond adequately to proper antimicrobial therapy; however, once an abscess has formed surgical drainage is requires. Ultrasonography or CT scan can be used to detect suppuration. Progressive induration, edema, and toxicity are also an indication for drainage.
Broad antimicrobial therapy is indicated to cover all possible aerobic and anaerobic pathogens, including adequate coverage for S. aureus, hemolytic streptococci, and beta-lactamase producing anaerobic gram negative bacilli. Many of the anaerobic gram negative bacteria causing these infections can produce beta-lactamase. 14 These include pigmented Prevotella and Porphyromonas as well as Fusobacterium spp.
Clindamycin, cefoxitin, chloramphenicol, imipenem, meropenem, the combination of a penicillin ( i.e. amoxicillin ) plus beta-lactamase inhibitor ( i.e. clavulanate ) or metronidazole plus a macrolide, will provide adequate coverage for anaerobic as well as aerobic bacteria. A penicillinase-resistant penicillin ( i.e. nafcillin ) or first-generation cephalosporin is generally adequate when the infection occurs is caused only by staphyloccoci. However, the presence of methicillin-resistant staphylococci may mandate the use of vancomycin or linezolid.
Prevention of suppuration can be achieved by early and proper therapy of odontogenic infections. A poor response in the treatment of Lemierre syndrome may require the need for anticoagulation, rather than for a change in antibiotics. However, the use of these agents is controversial.15 Because this syndrome is due to an endovascular infection, surgical draining of purulent collection (empyema, septic arthritis, soft-tissue abscess) is needed. Ligation and resection of the internal jugular vein is unnecessary in the majority of the cases.6
References
1. Beck, A.L.: A study of 24 cases of neck infections. Tr. Am. Acad. Ophthalmol. 37:342-381, 1932.
2. Reuben, M.: Postanginal sepsis: Report of 9 cases. Arch. Pediatr. 52:152-186, 1935.
3. Boharas, S.: Postanginal sepsis. Arch. Intern. Med. 71:844-853, 1943.
4. Lemierre, A.: On certain septicemias due to anaerobic organisms. Lancet 2:701-703, 1936.
5. Chase, S.: Infective thrombophlebitis secondary to neck infections. J. Iowa. Med. Soc. 25:252-259, 1935.
6. Sinave, C.P., Hardy, G.J., Fardy, P.W.: The Lemierre Syndrome: suppurative thrombophlebitis of the internal jugular vein secondary to oropharyngeal infection. Medicine (Baltimore) 68:85-94, 1989.
7. Goldhagen, J., Alford, B.A., Prewitt, L.H., Thompson, L., Hostetter, M.K.: Suppurative thrombophlebitis of the internal jugular vein: report of three cases and review of the pediatric literature. Pediatr. Infect. Dis. J. 7:410-414, 1988.
8. Moreno, S., Garcia Altozano, J., Pinilla, B., Lopez, J.C., de Quiros, B., Ortega, A., Bouza, E.: Lemierre's disease: postanginal bacteremia and pulmonary involvement caused by Fusobacterium necrophorum. Rev. Infect. Dis. 11:319-324, 1989.
9. Zimmerman, H.J., Fane, M., Utili, R., Seeff, L.B., Hoofnagle, J.: Jaundice due to bacterial infection. Gastroenterology 77:363-374, 1979.
10. Gudinchet, F., Maeder, P., Neveceral, P., Schnyder, P.: Lemierre's syndrome in children: high-resolution CT and color Doppler sonography patterns. Chest 112:271-273, 1997.
11. deWitte, B.R., Lameris, J.S.: Real-time ultrasound diagnosis of internal jugular vein thrombosis. J. Clin. Ultrasound 14:712-717, 1986.
12. Sanders, R.V., Kirkpatrick, M.B., Dasco, C.C., Bass JB Jr.: Suppurative thrombophlebitis of the internal jugular vein. Ala. J. Med. Sci. 23:92-95, 1986.
13. Yau, P.C., Norante, J.D.: Thrombophlebitis of the internal jugular vein secondary to pharyngitis. Arch. Otolaryngol 106:507-508, 1980.
14. Brook, I.: Infections caused by beta-lactamase-producing Fusobacterium spp. in children. Pediatr. Infect. Dis. J. 12:532-533, 1993.
15. Mitre, R.J., Rotheram, E.B., Jr.: Anaerobic septicemia from thrombophlebitis of the internal jugular vein: Successful treatment with metronidazole. JAMA 230:1168-1169, 1974.