This site was created by Itzhak Brook MD. It explains the diagnosis, etiology, medical and surgical (tonsillectomy) treatment and complications of tonsillitis ( tonsillar abscess, Lemierre's syndrome). Dr. Brook is a Professor of Pediatrics at Georgetown University Washington D.C.
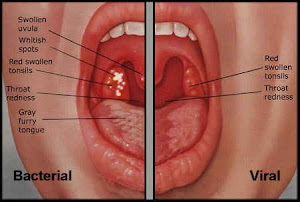
Tonsillitis is a common disease of childhood and adolescence. The diagnosis of tonsillitis generally requires the consideration of Group A beta-hemolytic Streptococcus (GABHS) infection. However, numerous other bacteria alone or in combinations, viruses and other infections and non-infectious causes should be considered. Recognition of the cause and choice of appropriate therapy are of utmost importance in assuring rapid recovery and preventing complications.
Penicillin is currently the first-choice treatment for GABHS pharyngotonsillitis. However, the growing failure of penicillin to eradicate GABHS is of concern. This website discusses the potential causes of penicillin failure ( i.e. the presence of beta-lactamse producing bacteria that can “protect” GABHS from penicillins) and methods to overcome them. It also discusses the role of anaerobic bacteria in tonsillitis and its complications.