This site was created by Itzhak Brook MD. It explains the diagnosis, etiology, medical and surgical (tonsillectomy) treatment and complications of tonsillitis ( tonsillar abscess, Lemierre's syndrome). Dr. Brook is a Professor of Pediatrics at Georgetown University Washington D.C.
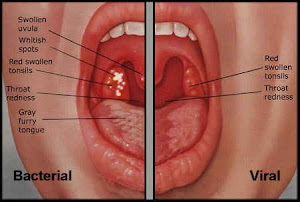
Tonsillitis is a common disease of childhood and adolescence. The diagnosis of tonsillitis generally requires the consideration of Group A beta-hemolytic Streptococcus (GABHS) infection. However, numerous other bacteria alone or in combinations, viruses and other infections and non-infectious causes should be considered. Recognition of the cause and choice of appropriate therapy are of utmost importance in assuring rapid recovery and preventing complications.
Penicillin is currently the first-choice treatment for GABHS pharyngotonsillitis. However, the growing failure of penicillin to eradicate GABHS is of concern. This website discusses the potential causes of penicillin failure ( i.e. the presence of beta-lactamse producing bacteria that can “protect” GABHS from penicillins) and methods to overcome them. It also discusses the role of anaerobic bacteria in tonsillitis and its complications.
Thursday, October 25, 2012
New guideline for the treatment of pharyngitis
Friday, August 17, 2012
Does Helicobacter pylori play a role in chronic tonsillitis?
Helicobacter pylori


.jpg)




